In blood donation, individuals willingly give vital tissue to be used for transfusion to themselves, a family member, or other persons in the general public. Blood transfusion is a medical procedure that is an important component of modern healthcare, saving countless lives every day. Blood transfusion involves the transfer of blood or blood products from one person (blood donor) into the bloodstream of another (blood recipient).
Anyone in good health can donate blood as long as they meet the requirements for the process. The requirements aim to avoid any complications that may arise for a donor or a recipient.

Courtesy: Red Cross Society
History of blood donation and transfusion
The history of blood transfusion and donation dates back centuries. English physician William Harvey performed the first recorded successful blood transfusion.
1628 – William Harvey, an English physician discovers the circulation of blood. This discovery allows for the first known blood transfusion to be attempted soon afterwards.
1667 – Jean-Baptiste Denis in France and Richard Lower and Edmund King in England separately report successful blood transfusions from sheep to humans.
1818- James Blundell, a British obstetrician, performed the first successful transfusion of human blood for postpartum haemorrhage management.
In the 20th century, significant advancements in blood typing and compatibility transformed blood donation & transfusion and the practice of medicine.
1901- Karl Landsteiner, an Austrian physician, discovers the first three human blood groups.
1907 – Ludvig Hektoen suggests that the safety of transfusion might be improved by cross-matching blood between donors and patients to exclude incompatible mixtures. Reuben Ottenberg performs the first blood transfusion using blood typing and cross-matching.
1939-1940 – Karl Landsteiner, Alexander Wiener, Philip Levine, and R.E. Stetson discover the Rhesus blood group (Rh blood group).
Blood Components and Functions
Blood is a complex tissue that contains several components and performs crucial functions. Donors can donate blood as a whole in whole blood donation (half a litre/ a pint), or they can donate components through apheresis (such as platelet donation (plateletpheresis), double red cell donation, and plasma donation (plasmapheresis)).
- Red blood cells carry oxygen throughout the body
- White blood cells fight infection
- Plasma, the liquid portion of blood, transports nutrients, hormones, and waste products
- Platelets are responsible for clotting, preventing excessive bleeding.
Types of Blood Donors
There is a classification of blood donors into voluntary donors, replacement donors, and paid donors. The three types of blood donors contribute to the blood supply, but they differ in their motivation and potential risks:
- Voluntary Donors: Donate blood out of altruism and a desire to help others, as there is no expectation of payment or reward. They receive a small token of appreciation with lunch or t-shirts. Considered the safest blood source, voluntary donors have less incentive to withhold information about their health history that poses risks to recipients.
- Replacement Donors: These donors donate blood to replace blood transfused to a specific friend or family member. They may face obligations or pressure from friends or family members to donate. This donor helps the recipient avoid some medical costs associated with blood transfusions. The eligibility and selection process may be less rigorous compared to voluntary donation, however, replacement donors might be less forthcoming about potential health risks to avoid being disqualified.
- Paid Donors: Receive financial compensation for donating blood. Payments are incentives given to the donors, so they donate more frequently, as this potentially increases the blood supply. Stringent screening processes are done, but the financial incentive may create a higher risk of some donors withholding crucial health information.
Blood Types
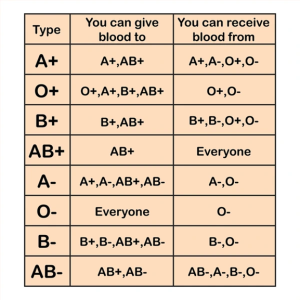
Blood types are classified based on the presence or absence of certain substances that trigger an immune response in the body (antigens). The blood type for each person is an inherited trait, passed genetically from your parents. Since some antigens can trigger a patient’s immune system to attack the transfused blood, safe blood donations and transfusions depend on careful blood typing and cross-matching. Humans have four major blood groups determined by the presence or absence of two antigens, A and B, on the surface of red blood cells. The blood groups are further classed based on the presence or absence of the Rh factor protein, which can be either present (+) or absent (–), creating the 8 most common blood types:
- A+ – A antigen on red cells with B antibody in the plasma, and a positive Rh factor
- A- – A antigen on red cells with B antibody in the plasma, and a negative Rh factor
- B+ – B antigen on red cells with A antibody in the plasma, and a positive Rh factor
- B- – B antigen on red cells with A antibody in the plasma, and a positive Rh factor
- O+ – neither A nor B antigens on red cells, but both A and B antibodies are in the plasma, with a positive Rh factor
- O- – neither A nor B antigens on red cells, but both A and B antibodies are in the plasma, with a negative Rh factor
- AB+ – A and B antigens on red cells, but neither A nor B antibodies in the plasma, with a positive Rh factor
- AB- – A and B antigens on red cells, but neither A nor B antibodies in the plasma, with a negative Rh factor.
Things to note are that the universal red cell donor in humans is Type O negative blood, and the universal plasma donor has Type AB blood. Universal recipients are AB+
Courtesy: Shutterstock Image
Process of blood donation and transfusion
Blood donations and transfusions typically involve several steps, beginning with the identification of the donor’s blood type through blood typing, as well as the recipients. This crucial step ensures compatibility between the donor’s blood and the recipient’s blood, minimizing the risk of adverse reactions. Blood donated can be used immediately or can be stored in blood banks in several healthcare facilities.
Once compatibility is confirmed, the blood is collected from a donor through venipuncture. The collected blood is then processed to separate it into its various components, such as red blood cells, plasma, and platelets. These components can be transfused individually, depending on the needs.
The transfusion is by infusing the blood or blood product into the recipient’s bloodstream through an intravenous (IV) line. Throughout the process, strict protocols are followed to maintain the integrity of the blood and ensure patient safety.
Requirements for blood donations
To be eligible to donate whole blood, plasma, or platelets, the World Health Organization recommends that:
- The donor must be in good health at the time of donation,
- The donor’s age is between 18-65, although policies may vary between individual donor centres and countries.
- Donors should weigh at least 110 pounds (about 50 kilograms).
- Donors must pass the physical and health-history assessments, and must not have recently travelled to mosquito-endemic countries, which means donors must be malaria-free, dengue-free, and Zika virus-free.
- A donor must not have engaged in “at risk” sexual activity in the last year (12 months).
- Donors should be HIV/AIDS negative, individuals should not donate blood if they have ever gotten a positive HIV test.
- Donors should never have used injected recreational drugs
- Pregnant women should not donate blood. Breast-feeding mothers are also advised not to be donors. Women who would love to donate can do so after pregnancy, and up to 3 months after weaning a baby.
Benefits of blood donation
Donating blood can impact positively on the donor’s health and well-being. These benefits include:
- Free Blood Screening: Blood donation involves a thorough health screening process, providing donors with valuable insights into their overall health and well-being.
- Decreased Risk of Heart Disease: Regular blood donation has been associated with a reduced risk of cardiovascular disease by lowering blood viscosity and reducing iron levels in the body.
- Sense of Fulfillment: For blood donors, blood donation can instil a sense of fulfilment as all blood donated would have a high potential of saving a life and as many as three lives according to the Red Cross Society.
Can persons with tattoos or piercings donate blood?
In some quarters, some years back, rumours spread about blood donation. People with tattoos or piercings were said to be ineligible for donations. However, in 2019, on World Blood Donor Day, a publication by the World Health Organization debunked the claim. In the publication, the organization stated “If you have recently had a tattoo or body piercing, you cannot donate for 6 months from the date of the procedure. If the body piercing was performed by a registered health professional and any inflammation has settled completely, you can donate blood after 12 hours. If you have visited the dentist for a minor procedure, you must wait 24 hours before donating; for major work wait a month.”
Conclusion
In conclusion, blood donors are a gift to society. If you meet the requirements, Wellahealth advocates for safe blood donation, as it shows altruism with enormous benefits. Your selfless act can have a profound impact on someone’s life!
To ensure you remain healthy and fit and join millions of other donors across the globe, Wellahealth provides affordable healthcare coverage, that ensures you and your family can become lifetime donors who save lives in no small way.
Contact Wellahealth today!
Dr Ifeoma Uduh, Dr John Afam