Introduction
Vitiligo is a skin condition characterized by the loss of pigment in skin cells, which can be a source of insecurity and raise many questions. It presents as light-coloured or white spots on the skin. It can affect people of all races but it tends to be more noticeable in Africans, Blacks, and those with darker skin tones.
The most common skin pigmentation condition is vitiligo. Researches show that about 0.1% to 2% of the world’s population is impacted. Locally in Nigeria, the prevalence of vitiligo varies from 2.8% to 6.6% depending on the region. Vitiligo usually starts in childhood or adolescence and peaks between 10 and 30 years, however, it can happen at any age. There are no racial disparities in the incidence rate, and both sexes are equally afflicted.
June is vitiligo awareness month and June 25th is World Vitiligo Day, this article aims to educate Nigerians on vitiligo, its causes, how it manifests, and current management strategies.
Source: Everyday Health/ Alamy/ Vittorio Gravino
What is Vitiligo?
Vitiligo is a skin disorder that develops when the melanocytes, which give your skin its colour, are destroyed. Affected skin sites become white or lose colour when melanocytes stop producing melanin, the pigment that gives skin its colour.
What causes Vitiligo?
The skin becomes milky white as a result of the immune system’s inadvertent attack on and destruction of melanocytes, the skin cells that give colour to the skin known as an auto-immune disease.
What causes the immune system to target skin melanocytes is unknown. However, research has shown that environmental triggers and stressful situations such as sunburn, emotional anguish, or chemical pollution exposure, can cause or exacerbate vitiligo.
Additionally, the Vitiligo Society also reports that there is a genetic predisposition to vitiligo, approximately 30% of cases have a family member with the condition. People with other auto-immune diseases (like systemic lupus erythematosus, psoriasis, pernicious anaemia, Addison’s disease, rheumatoid arthritis, thyroid disease, type 1 diabetes, etc) are also at higher risk of developing vitiligo.
Any part of the body might be impacted, and most vitiligo sufferers have multiple white patches. The same spot on both sides of the body, like your face, hands, or knees, may develop these patches. They may also emerge out of nowhere, taking up a significant portion of your skin and causing significant psycho-social problems.
Symptoms and Appearance of Vitiligo
White patches on the skin are the main indication of vitiligo. Often, you’ll see rapid pigment loss in several skin locations as the white patches may first appear unchanged and then enlarge over time as this may be seen in cycles of stability and loss of pigment.
Typically, these patches are:
- lustrous,
- hairless,
- symmetrical,
- clearly defined borders on both sides of the body (often)
Any part of the skin can be affected by vitiligo, but common sites include:
- the area surrounding the mouth and eyes (mucus membranes),
- both hands and feet,
- groin (genitalia),
- armpits,
- previously traumatized skin areas, and
- sun-exposed areas of skin, areas with moles
Other symptoms in those with vitiligo can also involve symptoms of other auto-immune diseases like:
- enlarged thyroid glands or a goitre
- low quantities of healthy red blood cells, or anaemia
- severe loss of muscle and weight
- early onset of grey hair
- sporadic hair loss
- fatigue and weakness.
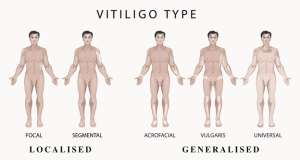
Types of Vitiligo
There are 2 main types of vitiligo:
- non-segmental vitiligo
- segmental vitiligo
Source: Vitiligo Society
Non-segmental Vitiligo
The symptoms of non-segmental vitiligo, also known as bilateral or generalized vitiligo, frequently manifest as symmetrical white patches on both sides of the body. There are several subtypes with distinct presentations known as:
- Focal vitiligo: The patches are usually smaller and limited to specific body areas. The patch often doesn’t change in size for a minimum of a year and a half.
- Acrofacial vitiligo: primarily affects the hands, face, and occasionally the feet.
- Generalized Vitiligo: Broad, symmetrical white spots spread over both sides of the body. It affects anywhere in the body’s pigment cells, this pattern is the most common presentation of vitiligo. Throughout a person’s lifespan, it frequently starts and stops numerous times. This is the most prevalent kind, along with acrofacial vitiligo.
- Universal Vitiligo: When vitiligo affects the majority of your skin and hair, it’s referred to as universal vitiligo. Usually starting as generalized vitiligo, it can eventually become universal. Universal vitiligo is an uncommon kind as at least 80% of your skin will become lighter if you have this.
- Mucosal vitiligo: This subtype primarily affects the vaginal or oral mucous membranes.
- Rare variations include follicular vitiligo (affecting hair), hypochromic vitiligo (affecting the scalp, face, trunk, and scalp; more common in persons with darker skin), and leukoderma punctata (tiny spots on the skin).
Segmental Vitiligo
Segmental or Localized vitiligo affects one side of the body, and only one side of the body develops white patches. It usually lasts between six and twenty-four months, after which it stabilizes, however, it might always start to progress again. It usually develops more quickly than Non-Segmental Vitiligo.
Management of Vitiligo
Even though vitiligo is not medically damaging, it can have a major negative mental impact on a person. The difficulties with self-esteem and the social stigma are serious issues.
Vitiligo has no known treatment or preventative measures. But you can improve the appearance of your afflicted skin. Depending on your age, the degree to which your skin needs to be improved, and the severity of your vitiligo, the medical course of action may vary.
Medications for Vitiligo
Medications used for the management of vitiligo include FDA-approved Ruxolitinib for non-segmental vitiligo in children greater than or equal to 12 years, topical corticosteroids, and calcineurin inhibitors. The corticosteroid creams have the potential to lessen inflammation and encourage the regeneration of pigment while the calcineurin inhibitors when applied to the skin reduce the activity of the immune system.
Ruxolitinib (Opzelura) cream has been approved by the FDA to treat nonsegmental vitiligo in adults and children 12 years of age and older as it has demonstrated success in repigmentation.
Therapies for Vitiligo
Phototherapy and depigmentation therapy are the two most common therapies employed in the management of vitiligo.
Phototherapy- also known as light therapy works by using UVA (ultraviolet rays-A) to either stop or decrease the spread of your vitiligo. This type of therapy is typically administered in a doctor’s office a few times per week.
Depigmentation therapy is the reduction of pigmentation on the skin. In cases where vitiligo has spread across a large portion of your body and previous treatments have failed, your doctor might suggest a depigmentation operation. This therapy aims to create uniform discoloration of skin, it eventually permanently lightens to blend in with the rest of your skin. It has several side effects including swelling, redness, dryness, and itchiness of the skin.
Other management protocol
- Surgery
- Skin protection:
- Use tanning treatments or makeup to cover the affected area of the skin.
- When you’re outside, wear sunscreen (with a minimum SPF of 30) and reapply it every two hours.
- Avoid using tanning beds.
- Refrain from being inked or tattooed as skin injury has the potential to worsen vitiligo.
Conclusion
Vitiligo remains the most common depigmenting condition of human skin, it has no known cause, it is not contagious, and does not cause cancer. However, it affects the psycho-social well-being of the person. Wellahealth advises that prompt diagnosis and treatment are crucial to ensure that a customized management plan suited for you is used for your condition speak with a dermatologist who has experience treating vitiligo.
This is why at Wellahealth Technologies, we recognize the value of all-encompassing medical treatment. Your ability to receive coverage for dermatologist visits, wherein they can diagnose and provide a customized treatment plan for your vitiligo, will depend on your particular Wellahealth insurance plan. Plans may also cover therapies or prescription drugs needed to treat the disease.
We invite you to look through our selection of Wellahealth insurance plans (starting from as low as #800/month) to see which one best meets your requirements. Send us a WhatsApp message to subscribe to the plan suited to your needs.
Dr. John Afam, Dr Ifeoma M. Uduh